- clinic
- March 10, 2020
- 58625
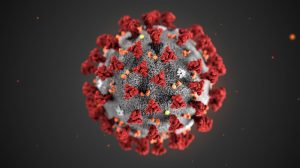
CORONAVIRUS AND DYSAUTONOMIA: WHAT YOU NEED TO DO NOW
Svtetlana Blitshteyn, MD
On February 29, 2020, I wrote an article, “Coronavirus and Dysautonomia: What You Need To Know” about coronavirus (COVID-19) basics and precautions as it relates to patients with dysautonomia and chronic illness in general. At that time there were only 3 cases of COVID-19 in the United States, but today we have more than 700 confirmed cases, and the number is rising; at least 26 patients died from COVID-19 in the United States.
If you feel your anxiety rising while reading this statistics or watching the news, know that you are not alone and that your concerns are valid. Recently, the infectious disease experts in the country recommended special precautions for people over 60 years of age and those with underlying health problems, such as heart or lung disease, diabetes or immunodeficiency. While many dysautonomia patients do not fall into these categories, having a chronic condition that affects the heart rate, blood pressure, digestion and temperature regulation could be considered an added risk to how an individual may be affected by an infection. Additionally, patients with autoimmune disorders may have altered immunologic response to an infection from the underlying autoimmunity, immunosuppressive therapy or both, which can result in a higher risk of complications and possibly a more difficult disease course.
While there is no data on how COVID-19 affects individuals with autoimmune and/or autonomic disorders, we can hypothesize how they would respond to COVID-19 based on their response to the flu. My personal opinion is that patients with these disorders should be viewed as high risk population even if the CDC and other organizations may not specifically identify them as such. To err on the safe side, I think it might be wise for patients with autoimmune and/or autonomic disorders to follow the CDC guidelines and infectious disease expert advice that’s applicable to people with underlying health problems or those over age 60. These recommendations are as following:
1. Try to avoid all activities that involve large crowds, such as concerts, conferences, large meetings, shopping malls, religious services and movie theaters.
2. Avoid all travel, especially by plane, both domestically and internationally.
3. If possible, work from home or attend school from home in order to avoid exposure to work areas and classes with many people.
4. Make sure you have enough medications that you take daily to last you a few weeks in order to avoid trips to the pharmacy.
5. Make sure you have enough food supply to last you a few weeks in order to avoid trips to the grocery store or restaurants.
6. Wash your hands with soap and water for at least 20 seconds thoroughly. If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol. If a hand sanitizer is not available at your local stores for purchase, you can make your own! See the Mighty article for easy recipes.
7. Avoid touching your face. If you have itchy or dry skin, use a moisturizer or anti-histamines to decrease itching.
8. If at all possible, people living with you in the same household should also follow these recommendations to decrease their chance of getting infected and passing it on to you.
9. While facemasks are not recommended by the CDC for prevention of COVID-19, you can certainly wear one if you have one and want to wear it, or if you wear one anyway due to mast cell activation syndrome or another condition.
10. Now is the time to discuss with your doctor how you can contact them if you are having a flareup of dysautonomia, or if you are sick with fever and cough. Your doctor may want you to stay home and not come to their clinic in order to avoid spreading any infection, whether cold, flu or COVID-19. Getting instructions from your doctor by phone, e-mail or video would be ideal in order to avoid the unnecessary trips to the doctor’s office, urgent care or emergency room.
Since the number of COVID-19 cases in the US is expected to rise in the next few weeks, according to the infectious disease experts, being cautious if you have a chronic medical condition is not only advisable, it is necessary to help decrease your chances of getting an infection. The single most important step you can do to avoid getting sick is to reduce face-to-face contact with people by staying home as much as possible over the next few weeks. While there is no need to panic, taking precautions to protect oneself based on medical facts is warranted, and being proactive can alleviate some of the anxiety associated with COVID-19 epidemic.
8 Comments
Thank you for your advice it is greatly appreciated
I greatly appreciate your article and wisdom. Due to this information, my employer has made arrangements for me to work from home.
Thank you!
👏
Thank you so much for this article. I needed to see it and I’m glad you are taking this serious.
Thank you so much for this information. It is exactly what I needed to know. I think I need to make smarter decisions starting today.
Thank you so much for this information. I was very anxious and this helped put me at ease.
Great advice thank you.
We live in Southwell, England. Our daughter has POTS and Asthma and we have isolated as a family from today as a precaution to help protect her. UK have low numbers of ICU beds and Ventilators so we have tough times ahead.
Our schools are still open but probably not for much longer.
Best wishes.
I believe my partner (age 68) and I (age 70) were ill with COVID 19 starting January 30, 2020. I still cannot get tested to see if I have a residual signature because we no longer are exhibiting most of the symptoms, and just still have a residual cough. I think we contracted the disease 3 days before in Napa at a winery or in Fairfield at a gas station.
We both had sudden and severe vomiting and diarhea for 8 hours. and I had to go to the ER in Grass Valley where we reside for IV fluids and medication. Then we had cold like sore throat, sinus and chest congestion. Our fevers were under 100, but the cough was deep and the fatigue completely debilitating for 3 weeks. Both of us have a low grade chronic asthma and breathing became very difficult. We get flu shots every year and rarely get ill. This illness was unlike anything we have ever experienced. We are concerned that we may still be infectious agents.
Comments are closed.